Our partners from HEIP provided us with a great analysis of the international access to drugs, especially for the developing countries. Learn more about HEIP Junior Consulting : www.juniorconsulting.heip.fr
Introduction and definitions
In 2000, following the Millennium Summit in New York, the United Nations (UN) established eight international developments goals, the so-called Millenium Development Goals (MDGs). All the 189 member states of the UN at the time and at least 23 international organisations committed to help achieve these objectives by 2015.
Each goal has different targets, four however are related to
health enhancement, (reference goal e.g. goal 4) solely relates to so-called developing countries (between 1990 and 2015)
Goal 4 : Reduce child mortality rates : reduce by two-thirds, between 1990 and 2015, the under- five mortality rate.
Goal 5 : Improve maternal health : reduce by three quarter, between 1990 and 2015, the maternal mortality ratio.
Goal 6 : Have acted by 2015 and begun to reverse the spread of HIV/AIDS ; achieve by 2010, universal access to treatment for HIV/AIDS for all those who need it ; have halted by 2015 and begun to reverse the incidence of malaria and other major diseases.
Goal 8 : Target 8E : In co-operation with pharmaceutical companies, provide access to affordable, essential drugs in developing countries.
MDGs were initially presented as the « minimal level of progress to achieve ». Brundtland, then Director General of the UN World Health Organisation named the priority : granting financings to achieve these objectives in terms of public health. According to this effort, the total amount of public-private partnership financings to the developing countries have been multiply by four between 2000 and 2007. The Bill and Melinda Gates foundation has single-handly given almost 900 billion dollar in 2012. From 2000, the global development aid amount raised by 61% in the period, while African countries received around 55% of these financings.
The misdemeanour of the pharmaceutical industry, qualified as « pharmagedon » (Healey, 2012) is a raising issue for public authorities, since they did not manage to organise theresearch. Drugs have become like every other products of consumption, large-scale produced and much advertised. Social studies often point the fact that health has nearly been integrated to « landscapes of consumption » (Curtis, 2004) free of ethical matters.
According to economists, drugs are of part of those kind of commodities that the market barely manage to regulate (Klimeck & Peters, 1995). As demonstrated by the enormous amount of needs from poor and developing countries, the supply is not adapted to this demand – and charity cannot solve this issue world-wide (Amat-Roze & Vaguet, 2012). In fact, philanthropy display a such important marketing campaign and concentrate the debate around itself, that it often hide other actions.
The situation is such that even the most greedy companies have no choice other than restore their image to their customer — however one might not forget that a huge part of this effort is only one communication matter, rather than actual commitment to global health (Dupont, 2013 ; Brulin, 2007 ; Vilaça, 2009).
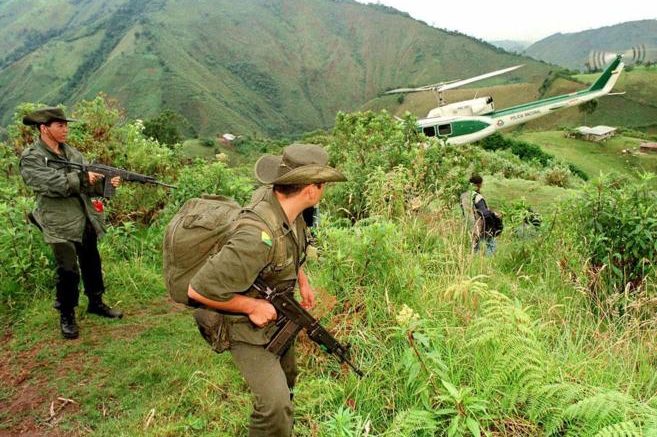
Regarding the current globalisation process and the development of the free-market on a global scale, this issue leads us more especially to consider the scope of intervention remaining for states — that logically appeared to be the main protectors their citizen’s health — to facilitate access of a great number of products from the private industrial companies. But in front of the competing forces on the globalised markets, are states and territories still meaning much ? In other world, we will question the complementarity between a marked out space, the territories, and a fluid space, the networks (Cummins, Curtis, Diez Roux & Macintyre, 2007).
On State level, the interactions regarding drugs begins with the Regulatory affairs (RA), also called government affairs, professions that are working with local, federal, and state regulatory agencies on specific matters such as ensuring legal authorisations, respecting sanitary norms and, and, of course, pricing the products. These king of interactions prove the impact of geopolitical issues on drug markets — influence of peddling, conflict between countries, competition…
Inequalities North-South : the Issue of Pricing
There are plenty different options in terms of pricing, from countries that ensure state regulations, to those that completely let the markets determining the rules, and with the issue public reimbursement and health care programs when they do exist.
(Sarmiento A.Z., Politique des prix des médicaments dans les Amériques, OMC report, « Economie de la santé et Médicaments », 1995).
In terms of health, we might replace the traditional distinction between developed and developing countries in : countries that pay for relatively expensive products (poor countries), and those that pay for cheap products, mainly because of health policies and socialised payment (rich countries). Of note, this distinction hides internal issues : for instance in Canada, drugs are the most expensive than everywhere, 35 percent of modest households cannot get what they have been prescribe (Babar, 2015).
Of course, the price variable cannot explain all the obstacles that make inaccessible to a third of the world population essential drugs (Vervasche, 2012). But this one variable may be the first effective lever for action to improve this delicate situation. This doesn’t fit the interests of pharmaceutical northern companies, that aren’t in accordance with a global downtrend — thus prices almost never stop increasing. Even worse, all the new speciality products (against hepatitis, or second generation antiretroviral drugs) experience strong price increase.
Here’s a comparaison by the WTO : http://erc.msh.org/dmpguide/index.cfm? search_cat=yes&display=yes&module=dmp&language=english&year=2014)
The Compulsory Licenses Regime
Yes, drugs cannot be invented by themselves. Research must be stimulated. However, does this need this widening gap between cost and retail prices ? One might consider this issue as the major impediment to drug access, in a world where open source has became a standard. 1995 was a pivotal year, when under pressure from the Western countries, the World trade organisation (WTO) instituted the Agreement one Trade-Related Aspects of Intellectual Property Rights (TRIPS), seeking to organise globally drugs trade. However, the strict respect of intellectual property bans drug copying for twenty years (Correa & Velasquez, 2009). In theory, this policy is, of course, useful to maintain the process of research and development that improve science and health. However, it’s interesting to see that, in practice, this measures permitted strict high prices and monopoly tendencies. Moreover, during the development phase, the pharmaceutical industry, for example in Switzerland, benefitted from the possibility to copy molecule from others (the Initiative for Medicines Access and Knowledge, I-MAK – a practice that is now forbidden)! So this principle of protecting discoveries benefits only to the same that created the TRIPS, the richest countries.
Trying to make the situation at least sustainable rather than equitable, the World Trade Organisation (WTO) proposed during the 2003 Doha round of negotiations, to set up a derogation system of patents : the compulsory licenses. This was suppose to allow public authorities to use a patent without any consent of the inventor and to run low priced products on the market for their population. However the Northern countries don’t actually use this principle so much, mostly because of their support to their laboratories. To restore their public image, the pharmaceutical companies prefer charity operation rather than giving licenses. It maintained the dependance of the South to Northern researches. The American diplomacy radically opposed the compulsory licenses and preferred bilateral treaties, like the TIPP (Transatlantic Trade and Investment Trade Agreement). For fear of trade retaliations, a lot of countries abandoned their project of licenses (Canada, Brazil, Thailand). However, India maintained its position on price dropping, using a compulsory license on an anticancer drugs.
Of note, the necessity, written in the Doha agreement, that the patent owner receive a proper remuneration, without any strict definition or any scale of remuneration. Also, no step has been taken on « fixed associations », the fact of assembling pills in one to make the treatment easier and cheaper.
At the end of the day, if the globalisation lowered the global prices for a large majority of commodities, mainly because the production has been transfer to places where salaires are lower (Krugman, 2000) and workers exploited, the same cannot be said on health drugs. Like the national level, the global scale didn’t change much, apart from monopolising communication campaigns, moral principles and charity calls have not been able to change much of this situation.
From an ethical point of view, one may consider high prices as equitable in countries where living costs are high. Logically, this would explain why research costs are charged on the Northern consumer more than other consumers across the world. However, the problem inferred by this system is that a great part of the research will be focus on diseases that affect a certain part of the world population, those that are solvent. This explains why there is less research on orphan diseases or on epidemics, as demonstrated the terrible episode of Ebola in 2014. This also explains why the countries that just opened their economy to the free market (largely because they have been asked to) are directly in a disadvantageous situation that prevent them to invest on drugs production.
Future Health ? Post-Western productions & Generic Drugs
We have entered a transitional period that may shape the future path we foresee global development. The golden age of pharmaceutical industries in the richest countries is behind. The global part of the five biggest companies dropped from 20 to 13% between 2005 and 2015, and the American companies part from 41 to 31% (IMS 2013). Moreover, most of these countries are about to loose exclusive use of their patents in the next few years, and will be concurrence by generic medicine.
We experience the first signs of the « post-Western world », starting with the high demand coming from low-income (mainly Sub-Saharan Africa). 17 « pharmerging » countries, China ahead, are moving into the lead of drug demand, passing between 2005 and 2015 from 12 to 28% of total drug selling. In parallel of this movement North-South, a shift is also happening on the products themselves.
In this new landscape of drug production, generic drugs will become much more present on the market : these products represent 39% of the total market today, while thy were twice less important ten years before. To adapt these economical reorganisations, the big pharmaceutical industries recently started to purchase asian companies, the ones they were fighting against few years ago.
On the field, generic drugs represent half of total consumption of low-income countries, when they have access to them (WHO, 2013). In fact this situation blow the first medicament prices up, sometimes multiply by 4. Among these generics, those that have the highest life-saving potential, the antiretroviral drugs are taking a prominent place.
These drugs have long been the archetype of global health scandals. Invented in the northern countries, these substances were of a high price, limiting their access to a large part of people suffering from HIV/AIDS. This situation was somewhat unlocked when « pirates » states proposed generic formulations.
At the same time, major companies, owners of the patents, proposed a modest decline in prices, the Indian private laboratories, like Cipla or Ranbaxi for instance, proposed a decrease of over 90% at the end of the last century. Today, for the production of 22 different antiretroviral molecules, there are as many industrials owners than generic industrials (Taverne, 2013, Descleaux, 2013). Regarding treatments against tuberculosis, the « Linezolid » from Pfizer, named Zyvox®, costs 15,000$ per patient for 6 months, whereas the generic version from Hetero, an Indian company, lowers the price by 90%.
Generics are often considered not as good in quality as the first drugs because it’s is produced in the developed countries, a rumour that has been clearly contradicted by the fast that 95% of production is made within the European Union (Imbraud, 2012). The quality issue is today a huge concern, but first and generic drugs taken together. The relocation of almost all the production to the low-income countries raise the issue of traceability in a divided system of production that multiply the number of subcontractors.
Pharmaceutical companies seek to present new patents without changing much the product. However, the southern countries are reacting more and more : in 2013, Indian Supreme Court turned down the patent projects of European and American companies on anticancer drugs.
STRATEGIST STATES & COMMERCIAL STRATEGIES
In March 2013, some associations defending people suffering from HIV/AIDS, like Positive Life or MSF, started an active campaign online against the European Union, accused of braking the transit of antiretroviral drugs and seeking to sign a bilateral treaty to reinforce the respect Intellectual property (IP) laws. Of note, the reaction of some major companies, that adapt themselves to this situation, like with the Dolutégravir (also called Tivicay) a treatment against HIV, that has been announced free of IP in the poor sub-saharan countries – a disposition negotiated with the UN.
However, this agreement did not include countries like Mexico, Brazil of Ukraine. More generally, this proved the great industrials remains upholders of the situation, and changes happened only when these companies decided to. Countries, and even more less-developed countries have almost no word to say. http://www.medicinespatentpool.org/medicines-patent-pool- et-viiv-healthcare-signent-un-accord-de-licence-pour-le-tout- dernier-medicament-anti-vih-ayant-ete-approuve-par-les- organismes-de-reglementation/?lang=fr
Case Study B : India, Crossroad of North and South
If India managed to find a different way to importation, it is thanks to the 1972 Patent Act, a weak IP legislation, which allowed an explosion of the private pharmaceutical sector (Rosary, 2009). The country is now the fourth largest drugs producer. However this fantastic development didn’t affect much the domestic health situation because almost 70% of the production of the biggest companies is directly exported to other countries, the favorite destination being the United States. The National AIDS control organisation (NACO) recognised that only half of the people suffering from this disease where receiving a treatment in 2013. The Indian state favours economical strategies rather than public health, even though it has the industrial capacity to act a lot more.
CASE STUDY 1 : INDIA, BETWEEN NORTH AND SOUTH ?
On the one hand, India is often considered as the « drugstore of the developing countries » because of its strong generic industry. On the other hand, half the population is still lacking access of life-important products. Every year, 63 million people are dropping down the poverty line trying to get health care. A governmental report from December 2014 said « the cost of care access are one of the first factor of impoverishment of the population, like never before ». Inexistant social security and limited private medical insurances explain why the country as one of the most important medical spendings rate per capita.
Despite the high prices, the Supreme Court announced in 2015 that price fixing policies were « unreasonable and irrational ». They preferred letting the market run wild with competition between companies. According to the liberal perfect competition guideline, this decision would allow price dropping. However, in India, where there is not the culture of patents, the choices of the products is based on a distinction between brands, not on the biological constitution and the same molecule can be sold in variable prices, which is not in favour of the consumer. Moreover, recent studies determined the impact of pharmaceutical companies on Indian doctors, those that prescribe the drugs to the patient. This is due to the lack of a legal frame and weak independent institutions (Gourou, 1982). For instance in Pakistan, studies estimated that 90% of doctors prescriptions are still oriented by brand drugs. The second issue is the weight of counterfeit drugs, that represent a quarter of the total Indian drug market (« Fake and Counterfeit Drug in India. Booming Biz », Assocham, 2014). Because of the large number of copies, the Indian average consumer need to buy the most expensive brand to avoid counterfeit. If the government was able to secure the market by guaranteeing the quality of available drugs, in particular generics, their would be much less domestic spending on health matters. If generics are dropping the prices, by at least 48%, (sometimes by 80% !) depending on studies, the introduction of this kind of products raise concerns on their quality. Governmental regulation has to the intermédiaire between production and distribution, of course when institutions aren’t corrupted or influenced in one way or another. Today, there is only 300 inspectors for 10,000 laboratories in the country. This lack of governmental action has dramatic consequences. Between 2008 and 2013, 7,800 patients died in the 48 hours following a treatment in the Jammu and Kashmir public hospital because of counterfeit copies. The bad material conditions also affect the availability of health products : the shortage of electricity in the rural part of India prevent the preservation of drugs.
Confronted with this issue, the Indian government announced in February 2016 that it will provide insurances to the poorest households, that would finance heath spendings to the amount of 1,300€. At the same it reduced public spendings on health to 1% of the GDP. This decision raises interrogations on whether or not the situation is about to change. Beside quantity, scholars pointed out another issue. Since developing markets are asking for cheaper prices above all else, manufactured drugs quality lowered in recent years (Videau, 2007). Nothing would change if any legal sanitary ground is not set up, if no independent regulatory agencies are created and if governance remain split up between state authorities, private companies and non-governmental actors.
Case Study B : Raising Concerns & the Dependance of African Countries
The less-advanced countries (34 are Africans) that barely have sufficient industrial infrastructures and financial means to develop their pharmaceutical sector, count on imports and eventually depend on charity. With the compulsory licenses granted by the WTO, they can start building local dispositions. But the one problem remains: which company would like to invest in countries that cannot pay their high prices? For the moment, transnational are not hurried to invest in these countries that represent only 1% of World trade. They may not have the chance to benefit from these WTO advantages that are limited in time. Ouganda is one of the rare example of a country that launched its national industry because of these facilities.
Part of the BRICS, South Africa’s health situation is not much better than the rest of the continent. Take the illustrative example of the Trastuzumab, a treatment against breast cancer, that won’t be available to generics production until… 2033 ; whereas already available in other countries like South Korea. The actual drug is thus very expensive in the country : it would cost around 28,400€ per year, whereas 8,850 in India (Le Monde, 2016).
The numerous patents for medicines against HIV/AIDS, cancer, hepatitis, diabetes, epilepsy or malaria protect the major companies and avoid any further improvement of the health situation in this country, which is dramatically, but logically, the most touched (per capita) by AIDS.
Lotti Rutter, from the NGO Treatment Action Campaign (TAC), explains how lax the government is regarding patent issuing, without caring about whether or not it’s justify (Le Monde, 2016).
A recent study from Pretoria University (2011) estimated that 50% of patents wouldn’t have been granted if the patent application had been examined meticulously. In fact, according to the government, 2,442 patents have been issued in 2008 in South Africa, whereas only 278 have been granted in India for five years, during 2003 and 2008.
The local newspaper Mail and Guardian revealed in 2014 the extend of the pharmaceutical lobbying on South African government and institutions. Moreover, the US and the European Union pushed forward the respect of Intellectual property, especially by giving subventions to maintain the situation — without any concerns on the bad health situation in the country.
But this status quo is about to change, due to the willingness of governments, un addition to the role of the civil society. Of note, the victory of South Africa against 39 major laboratories that were against the introduction of generics in the country. Starting for this point, the government of Jacob Zuma succeed in granting free access to antiretroviral treatment to 3,4 million HIV-Positive people among the 6,4 million that count the country.
The 21th century will experience the emergence of transnational actors. They opposed two kind of actors : on the one hand, militant, groups of pressure and NGOs, that emphasise the ideas of justice and equality ; and on the other hands, transnational companies, that are following neoliberal guidelines. The latter is more and more followed by international institutions. This theoretical tension between liberty and justice may be the global issue of the following century, not only in terms of health.
On the field this is no equitable fight, even if some countries like Brazil or India start opposing the status quo and the powerful states (USA). This situation hides major concerns on less-developed countries such as the degree of manipulation of the market by the pharmaceutical industry. Regarding this issue, there is not actual proof of these kind of actions by companies. There is however highly suspecting studies that affirm that we had the possibility to cure major disease like HIV/AIDS, or at least to contribute to stop the progression world wide, if it wasn’t unrentable.
In the case of malaria, some researchers found the way to cure the disease that affect 3,2 billion people, almost half of the population, with a plant infusion, the artemisia, that is completely natural, easy to crop, not expensive at all and more efficient than aggressive and expensive traditional ACT (Artemisinin-based combination therapy) drugs. These scientists insisted, in a report issued in January 2016, on the pressures they received to stop their studies — some researcher have even been poisoned (More for Less & Artemisia, 2016).
Conclusion
For now, facing glaring drug access inequalities, all initiatives have failed to establish a sustainable situation equitably setting a price and quality of health products in the world. Palliative facilities only permitted to start reducing the most outrageous public health situations, nothing more — and the future remains highly uncertain. One can not expect too much from the states : most of them remain far too weak and the Triad members are still controlling most markets. Well beyond what can governments, long term initiatives shall come from multilateral actors. WHO experts noted in 2013 the difficulties of the patent system to stimulate research towards the needs of people in the least developed countries, those in need. They proposed the creation of an international convention to secure research fundings toward new drugs. This proposal jeopardises the argument put forward by the pharmaceutical industry to justify high prices to supply the process of research and maintain jobs. National contributions to this international fund would be calculated based on the level of wealth of each country. In a way, this would be an a global initiative, thanks to its sustainable financing mode and the introduction of the concept of « common goods » as an alternative to patents and as a part of the Amartya Sen’s definition of « capabilities ».
There is also the idea of abandoning drugs patents and letting free access to the researcher results (open source), which raises other concerns : not only in terms of health, is a system based on the notion of individual profit sustainable ? There’s a long way to go towards better governance and transparency, not to mention universal access to the benefits of science.